From the MTASA (Massage Therapy Association of South Africa) Conference 02 June 2023, lecture notes taken by Roxanne, from the lecture by Registered Podiatrist – Lucas Breedt.
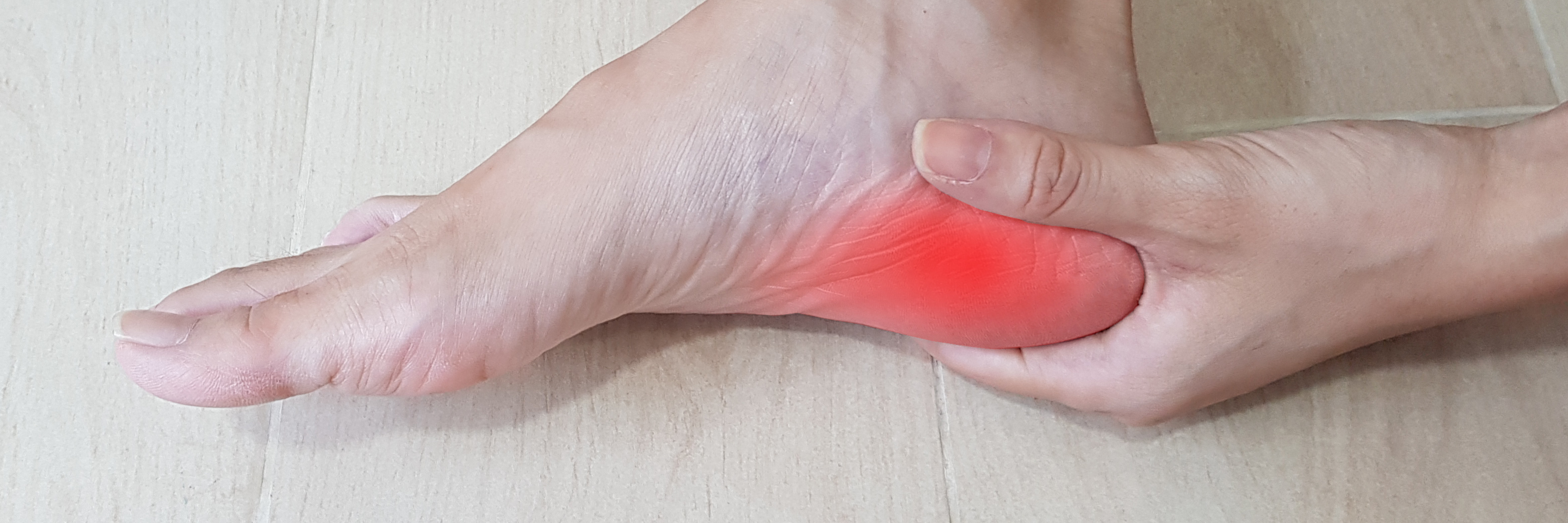
Are you suffering from recurring heel pain?
The plantar fascia (PF) is a robust structure consisting of fascia and aponeurosis elements. It connects the heel to the toes, stabilises the metatarsal bones, assists in shock absorption and forward propulsion. The PF offer as a stabiliser for the foot arch, and turns the foot into a rigid lever to move forward.
The aponeurosis function is similar to a tendon, both attach muscles to bones, when you move your muscles, the aponeurosis acts as a spring to endure the tension and extra pressure. It absorbs energy when your muscles move. Aponeurosis gives your body strength and stability, it acts like another type of connective tissue called fascia. Fascia is fibrous tissue that wraps around and supports your muscles, organs and bones.
Anatomy:
Origin: medial tubercle of the calcaneus (heel) and Insertion: medial, lateral and central bands (fascial component).
Central band: (aponeurosis component) branches off into 5 sections which insert into the phalanges (toe bone) via their respective plantar plates.
Vascular component: branches off the posterior tibial artery (feeds the plantar components), branches off the dosralis pedis artery (feeds the dorsal components).
Neurological components: supplied by the medial and lateral plantar nerves. The neural component is linked to the pain that the client feels.
The Windlass Mechanism: this is an engineering term which comes from the explanation describing when a cord or structure wraps around a poll, and the pull that it has on it. Dorsiflexion (lifting up) of the hallux (big toe) during the propulsive or toe-off phase of the gait (walk) cycles causes the fascia to unwind around the 1st metatarsal head. – This is the correct way for the structures of the feet to respond when walking.
The Inactive Windlass Mechanism – this describes when the fascia is always tight, this causes tension with compression and when the weight is being put on the foot. This causes the foot to inwardly rotate instead of outwardly rotate. – Correct biomechanics would have the foot rolling outwards instead of inwards.
Pathomechanical issues caused by PF: excessive traction forces, overpronation – foot flexor weakness and intrinsic muscle weakness, gluteal region muscle imbalances (the gluts may be very tight, affecting the foot – the gluts stabilise the knee and externally rotate the foot), subtalar joint axis position (medially deviated) – the joint runs through the calcaneus and through the talus – if it is out of alignment it causes the foot to lock up the first metatarsal joint for less dorsiflexion so the foot can’t rotate outwards properly. Foot posture (flat feet or high arch), forefoot stability and hallux rigidus/limitus. Glut weakness – can cause the feet to evert and point outwards – walking like a duck and inner knee pain.
In PF there is plantar tearing at the start of the fascia – which is at the end of the heel (before the start of the arch under the foot), there isn’s as much pain felt along the rest of the fascia but rather is more centralised around the heel.
Pathophysiological factors: There is healthy inflammation in the body (it is acute inflammation which helps the body to heal, it has a vasodilatory effect, stimulates a tissue/immune response – which provides resolution and overall recovery which leads to cellular and tissue homeostasis. After a treatment it is normal to have a flair up of inflammation, and it is important to note that it assists in the recovery) and unhealthy inflammation (this is caused by excessive inflammation which turns into chronic inflammation – this may cause and excessive immune/tissue response which results in the failure to resolve the problem (from repetitive damage) – the cycle becomes bigger and bigger and bigger which leads to a chronic inflammatory disease – this can happen within 72 hours of the injury). The main goal is to reduce the cycle of inflammation.
PF – the pain is worse when standing up in the morning, after exercise and after rest. It is most likely caused from a mechanical deficit. On the day of the injury there will be a healthy inflammatory response. Doing the same repetitive movement that is causing the PF results in an unhealthy inflammatory phase.
Treatment: Is it Fasciitis – acute inflammatory stage of condition – first 48 hours after pain occurred? OR, is it Fasciosis – refers to the degenerative stages of the condition (can start to occur within 72 hours of injury) – there is now thickening of the fibrous bands and changes in the collagen – the client complains that their feet are always sore. The tissue becomes more fibrous (there is a cycle of damage and degeneration).
Management in fasciitis stage: RICEN (Rest, Ice, Compression, Elevation and Non-steriodal Anti-inflammatories). Principle: reduce inflammation, mobilise tissue passively – passive stretching (calf muscles – stretch for 10 seconds at a time), mobilise foot flexors and posterior kinetic chain, offload and support fascia as much as possible and avoid further irritation to the area (avoid deep heat and rather go for ice to the area).
Management of fasciosis stage: Mobilise the posterior kinetic chain, strengthen muscles deficits, load the fascia (strong and deep massage) – by also working out the gluts and putting load on the achilles tendons, address gait abnormalities, apply mechanical offloading, injection therapies and surgery. Injections: Cortisone – may help the pain but doesn’t resolve the problem, only required if the client needs a very quick result for a specific event or for travelling. Injections – PRP uses the patients own platelet-rich plasma injections into the area, their is a massive inflammatory response there and can be quite painful for the client.
Why treatment might fail? Determine if the patient is in a fasciitis or fasciosis stage. Was the correct structure treated? Are there secondary or tertiary conditions inhibiting recovery (e.g. bunions or heels spurs)? The presence of chronic diseases or malignancies / PF is prevalent in a woman’s second or third pregnancy / patient’s compliance / correct rehab protocols followed and footwear.
Therapeutic Massage is a proven effective treatment of PF in many cases, your therapist will do a thorough consultation with you to determine the possibility of good results from your treatments, and the most suitable treatment plan for effective results.
For more information, bookings or for enquiries, please contact Roxanne on WhatsApp: 079 567 5090.